
Lumbar spinal stenosis
Definition :
We speak of a spinal stenosis, when the space available for the nerves is too narrow. By extension, we also often group together under this name the foraminal stenosis (the small lateral exit holes of the column) and the recessi stenosis (the bend that the nerve takes before leaving the column).
Classically, there are 3 types of narrow lumbar canals:
-
Congenital (related to short pedicles)
-
Degenerative (linked to joint hypertrophy)
-
Mixed (combining short pedicles and joint hypertrophy)
Several main elements will contribute to increasing the stenosis (narrowing) of the narrow lumbar canals:
-
Disc protrusion (as this is a degenerative injury, the disc has often degenerated as well and therefore lost its height. Loss of disc height results in protrusion because the posterior longitudinal ligament is attached to the adjacent vertebrae, but may wrinkle next to the disc. This element will be classically dynamic, ie it will increase in lordosis and decrease in kyphosis).
-
Indirect foraminal stenosis (also linked to the loss of disc height, therefore also dynamic).
-
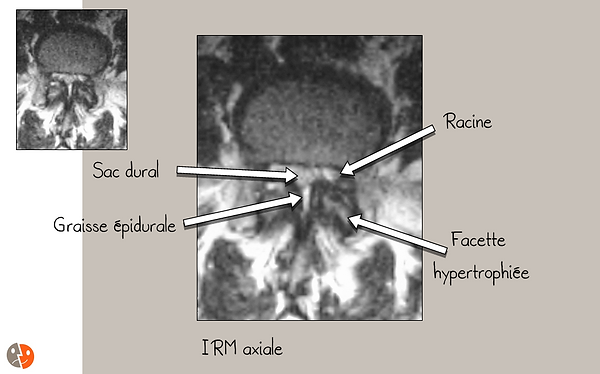
A " hypertrophy of the yellow ligaments " (in fact, it is the approximation of the insertions of the yellow ligaments in case of joint hypertrophy which makes them thicker). Measuring the area of the spinal canal using only the bony boundaries is therefore meaningless and it is the area of the dural sac (in an axial section) that takes on more significance.
-
A yellow ligament cyst . These cysts are more common in cases of joint enlargement and increase the degree of compression.
-
Epidural lipomatosis . These lipomatoses are more frequent in the case of a narrow lumbar canal and increase the posterior compression on the dural sac.
-
Spondylolisthesis (sliding of one vertebra in relation to another). Degenerative spondylolisthesis will increase ductal stenosis and may affect the technical choices in the event of an operation depending on its stability.
-
Associated scoliosis will increase the stretching of the roots and their sensitivity to compression on the one hand and on the other hand increase foraminal stenosis in the concavities .

Clinical features:
-
Neurogenic claudication
-
Unilateral, bilateral or toggle
-
Usually without neurological deficit
-
Decreased by anterior flexion of the trunk and sitting position
(We always ask if the patient is relieved by pushing a cart when shopping in supermarkets) -
Differential diagnosis with a vasculary origin
-
-
Low back pain (contrary to popular belief, a narrow lumbar canal can only manifest itself as low back pain without any root component)
-
Limitation of the walking perimeter . Finally, this element is the most important, because the pain remains subjective by definition and some patients hardly describe pain even though they are unable to walk more than 200 m without stopping. The functional impact is more significant than the pain.


Operative indication:
-
There is no absolute indication for operation because it is the impact on the patient's quality of life and autonomy that is decisive. As guidelines, we can retain:
-
Pain deemed disabling by the patient
-
Walking perimeter less than 1 km (below, massive atrophy of the musculature tends to occur)
-
Loss of independence / autonomy (like pain, this is highly subjective)
-
-
There is no real age limit, because the morbidity / mortality linked to reduced walking in the elderly often exceeds the morbidity / mortality linked to the operation.

Lumbar spinal stenosis: Radiological evaluation
Radiological evaluation:
-
Functional lumbar x-rays under load
-
Lumbar CT scan

Lumbar CT-scan:
-
Shows bone and osteoarthritis very well
-
Shows the yellow ligaments well
-
Shows the dural sac moderately well
-
Shows good disc protrusions
-
Requires a large dose of rays because must be carried out continuously on many levels to assess the cranio-caudal extension of the stenosis.
-
Requires sagittal reconstructions to properly assess foraminal stenosis and any associated slips
Lumbar radiculography:
-
Invasive examination
-
Remains the "gold standard" in certain difficult cases
-
Shows well the central stenosis and recessi
-
Must be combined with a post-radiculography CT-scan to fully appreciate the yellow ligaments, the disc and the facet joints
-
Can be combined with dynamic images (in flexion / extension), which has the advantage of clearly demonstrating the dynamic component




Lumbar MRI:
-
Non-invasive examination
-
Good vision of the roots, the dural sac
-
Assessment of the state of hydration of the disc and indirect signs of its degeneration (Modic signs)
-
Assessment of the entire lumbar spine
-
Assessment of the paralumbar musculature
-
Possibility of myelographic sequences simulating radiculography to some extent
-
Limited visualization of osteoarthritis
Canal lombaire étroit: Traitements
Treatment options:
-
Abstention
-
The narrow lumbar canal does not have enough functional impact or does not cause "enough" pain
-
The patient's comorbidities make the operation too risky from an anesthetic point of view
-
Philosophical choice of the patient (because of his age or any other consideration)
-
-
Conservative
-
There is no real conservative treatment, but physiotherapy and occupational therapy can nonetheless help the patient to live better with their narrow spinal cord. Several elements can contribute to this clinical benefit:
-
Accept the posture of anterior flexion of the trunk which relieves the patient. For example, pushing a cart will relieve it, as will walking with a rolator.
-
Make those around them accept the postural disorder in anterior flexion of the trunk! How many times will the patient hear "But sit up! It's better for your back!" and try to do it while it increases the pain?
-
Learn to divide your activity. It is consecutive time that causes pain, not cumulative time. The patient will not be able to walk 60 minutes at a stretch, but will be able to walk 4 x 15 minutes or 6 x 10 minutes.
-
Maintain the best possible lumbar musculature by going for a fractional walk (it seems that good paralumbar musculature slows the progression of osteoarthritis).
-
Go up the floors (because the position is favorable), but go down by elevator (because this increases lumbar lordosis which worsens the compression of the nerves).
-
Avoid a static standing position which increases lumbar lordosis (therefore avoid aperitifs, exhibitions, concerts, etc.). For example, if the patient meets a friend on the street, he should not stop to talk to him, but either suggest that he sit down to chat or talk while walking.
-
Avoid sleeping with your legs stretched out and always put a cushion under the knees to sleep on your back (because bending the knees decreases lumbar lordosis).
-
Core exercises are useful, but often difficult to do after a certain age. However, some simplified exercises can be performed.
-
-
-
-
Epidural injections : Historically, epidural injections were quite popular for patients suffering from a narrow spinal canal especially multistage as it allowed an effect on many roots. There are several major flaws with epidurals in case of a narrow lumbar canal:
-
Volume effect: the injected product takes up space in the channel which is by definition too narrow, resulting in increased compression (often transitory however)
-
The risk of dural breach is increased because the space between the yellow ligament and the dura (epidural space) can be virtual and the injection technique with loss of resistance can become very random.
-
The distribution of the injected drug is sometimes quite random and an epidurography is required to assess it. Epidurography unfortunately has the consequence of increasing the intracanal volume effect.
-
The approach can be made technically difficult due to the facet hypertrophy and potentially the hypertrophy of the spinous processes. The use of fluoroscopy is imperative.
-
From our point of view, epidural injections are not indicated in cases of narrow lumbar duct unless epidural lipomatosis is associated.
-
If an epidural is done, two things can reduce the risk:
-
paramedian approach (which makes it possible to better avoid the articular facet and the spinous membrane and reduces the length of the needle which will pass into the epidural space).
-
prone position rather than lateral decubitus as this further relaxes the dura and slightly increases the epidural space which limits the risk of dural breach (but increases root compression, which can be painfully felt by the patient)
-
gesture performed under sedation to avoid any untimely movement of the patient and reduce pain (which decreases the Valsalva effect and dilation of the dural sac, thus reducing the risk of dural breach).
-
-
-
Facet blocks : Bundle branch block type facet blocks have very little effect on patient pain and no effect on walking perimeter. Intra-articular facet blocks often have a good effect on the patient's pain, but this is limited in time (on average 1 to 2 months). Iterative intra-articular facet blocks are probably the best alternative for patients who cannot be operated on due to their co-morbidities or for those who do not want to be operated.
-
Periradicular blocks : Periradicular blocks have no real application in narrow lumbar canals due to their exclusive extra-canal effect.
-
-
Operations :
-
It is an eminently "tailor-made" surgery because no two narrow lumbar canals are strictly identical. Many elements associated with the narrow lumbar canal will influence the technical choices (spondylolisthesis, scoliosis, cyst of the yellow ligament, etc.)
-
The main surgical choices are:
-
Decompression (laminectomy, foraminotomy, arthrectomy, unilateral or bilateral, ...)
-
Spondylodesis (PLIF, TLIF, posterior graft, instrumentation, ...)
-
Dynamic stabilization (interspinous, instrumented, ...)
-
Pure analgesic (morphine pump, spinal cord stimulator, ...)
-
-
The surgical options mentioned above can be combined, so the possibilities are almost endless.
-
Due to the very numerous surgical possibilities, the heterogeneity of the basic pathology and the long course, no truly valid prospective randomized study can be carried out. The patient will therefore receive multiple and discordant opinions depending on the surgeons he will consult.
-
Lumbar spinal stenosis: Operations


Bilateral decompression:
Bilateral decompression is the "classic" operation for a narrow lumbar canal. It can be carried out on one or more floors. Several elements are included in this decompression:
-
Bilateral laminectomy (complete blade removal) or bilateral hemilaminectomy (partial blade removal)
-
Bilateral flavectomy (removal of the yellow ligaments)
-
Spinectomy (partial removal of the superior spinous process and the inferior spinous process) with removal of the interspinous ligament
-
Partial facet arthrectomy (by submining to decompress the foramina as much as possible (middle part) and recess them without too much compromising the stability of the segment)

Preoperative CT-scan:
The part removed during bilateral decompression is stained. It is:
-
The blades
-
The thorny
-
Yellow ligaments
-
Part of the facet joints

Operative view:
This is a view taken through the operating microscope. The dural sac is well decompressed and has taken on a cylindrical shape. In real view, we also notice that it pulses with the heart rate and with the respiration testifying to the absence of residual compression.
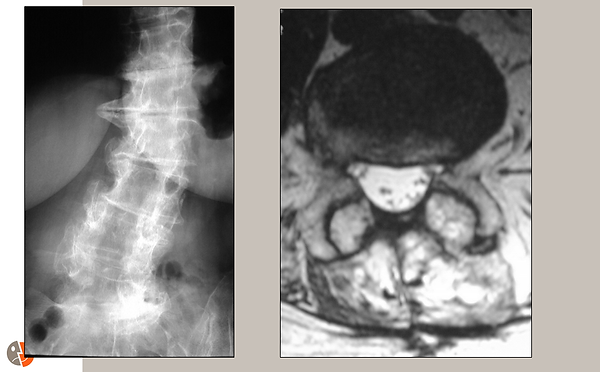
Postoperative x-ray and MRI:
The image on the left is a frontal x-ray showing decompression (dark area) over several stages. Scoliosis is also well demonstrated.
The image on the right is an axial MRI slice. The decompressed dural sac is visible in white.
Possible complement to decompression: Spondylodesis
Lumbar stability after decompression is a subject of great controversy.
Depending on the type of decompression, instability will be created particularly if stabilizing structures such as the interspinous ligament or the facet joints are sacrificed. Elements intrinsic to the patient's spine will also influence this stability such as spondylolisthesis, scoliosis, disc degeneration or poor quality of the paralumbar musculature.
Two combinable philosophies aim to reduce the risk of postoperative instability:
-
Decompression "nuanced" to less destabilize. For example, one can opt for unilateral decompression thus preserving the interspinous ligament, the yellow ligament and the contralateral facet joint. You can also open only the foramina and recessi. There are many variations and technical nuances (the use of rapid burs and the surgical microscope allows more important structures to be preserved)
-
Spondylodesis : A bone fusion with or without posterior instrumentation will prevent instability of the operated segment. An intradiscal cage fusion may be a less invasive alternative. Several elements must be taken into account in the choice or not to perform a spondylodesis:
-
As these are often elderly patients, the increase in the duration of the intervention and the bleeding (consequences of associating a spandylodesis) increase the morbidity / mortality of the intervention. Sometimes, a sequential approach can be less risky (2 operations of 2 1/2 hours are less risky than a 5 hours operation in an elderly patient).
-
Too much rigidity in the operated segment increases the risk of destabilizing the adjacent segments. The choice of material used for spondylodesis will influence this risk by modulating the elasticity of the assembly.
-
The cost of the intervention is considerably higher. The risk of having to operate again if a spondylodesis is not performed must of course also be taken into account.
-
A non-dogmatic and individualized approach to narrow lumbar canal surgery therefore seems to us the best way to proceed.
Lumbar spinal stenosis: Dynamic interspinous stabilization
Surgical alternative: Dynamic interspinous stabilization
Dynamic interspinous stabilization can be used as a single operation or as an adjunct to decompression as long as the spinous processes have been preserved as well as sufficient blades.
The principle is to indirectly open the foramina and prevent them from closing in lordosis.
If the patient feels an improvement in anterior flexion of the trunk, there is necessarily potential for improvement for dynamic interspinous stabilization as this simulates anterior flexion of the trunk (lumbar "delordosis").
Interspinous impants:
There are many interspinous implants (Diam, Coflex, Aperius, X-Stop, GelFix, ...). Some are designed for percutaneous implantation while others need a more classic opening.
All implants have elements designed to prevent their migration out of the interspinous space.
Lumbar spinal stenosis: Postoperative physiotherapy



Lumbar spinal stenosis: Instructions for future patients
These instructions concern patients operated on by our team. Each center has its own treatment protocols and they may differ from the instructions below.
Preparation before the operation:
-
Anti-aggregating drugs like Aspirin or Plavix must be stopped 10 days before the date of the operation. However, you must make sure with your doctor or your cardiologist that this stop is not risky. If a stop is not possible, you should inform your surgeon and your anesthesiologist to see if the planned operation is being continued on the planned date.
-
Anticoagulant drugs like Sintrom should be stopped 1 week before the date of the operation. Crossbreeding with heparin injections (eg Fraxiparine, Fragmin) will be performed under the supervision of your attending physician. A 60% PT is required for the procedure. However, you must make sure with your doctor or your cardiologist that this stop is not risky. Modern anticoagulant drugs like Xarelto should be stopped 2 days before the date of the operation. If a stop is not possible, you should inform your surgeon and your anesthesiologist to see if the planned operation is being continued on the planned date.
-
You should bring a list of your usual medications for the procedure. If your treatment is not common, consider taking the medicines themselves as well.
-
You must bring your last radiological examinations (CT, MRI, X- rays ) for the operation if you have these at your home.
-
In the event of a known allergy , please inform the nursing team and the anesthesiologist even if it is already in your file. Certain allergies may require a specific allergological assessment and lead to postponement of the procedure.
Postoperative consequences:
-
Keep the position in bed on your back for 4 hours to facilitate hemostasis, then you can turn onto your side en bloc.
-
In the absence of cerebrospinal fluid leakage, it is not only possible but desirable to get up and walk as early as 6 hours postoperatively. You must get up as a whole and the physiotherapist and / or the nurse will accompany you for the first awakenings.
Wound - scar:
-
The scar will be more beautiful if it is not exposed to the sun for 1 year after the operation. Remember to protect it either with clothes or with a total screen.
-
Steristrips should be kept until check-up 3 weeks postoperatively.
-
The threads are absorbable and do not have to be removed .
-
In case of discharge and / or fever , please call the secretariat immediately (021 923 3848) or in case of unavailability your attending physician, the hospital where you had the operation or the emergency department of a hospital near your home.
Drugs:
-
The usual medications should be continued as before the operation.
-
Anti-aggregating drugs such as Aspirin or Plavix can be resumed the day after the operation.
-
Anticoagulant drugs such as Sintrom can be resumed as early as 3 days after the operation.
-
Analgesic drugs (Dafalgan, Irfen, Tramal, etc.) should only be taken in the event of pain; they are not compulsory and do not influence healing in the proper sense.
Return home:
-
Remember to take your radiological record with you when you return home.
-
Please check that you have enough medication at home for the day of your return, especially before a weekend or holiday.
-
Please check that you have received (if necessary):
-
prescription for pain medication
-
the prescription for physiotherapy (not systematic)
-
the order for the caregiver at home (make contact before the intervention)
-
work stoppage
-
the date and time of the next check-up
-
Physical activity:
-
Walking is the best physical activity after such an intervention . In the absence of pain, no time limit is set. It is however preferable to privilege the frequency to the duration. Thus, it is generally better supported to walk 4 x 15 minutes per day rather than going for an hour-long walk per day.
-
Heels between 1 and 4 cm are most suitable for the back.
-
You must respect the limits dictated by your body , because an excess of activity one day almost always leads to a limitation of the activity on the following days with a negative overall balance.
-
Historically, a limit for loads was systematically prescribed. We currently believe that overhangs should be avoided as much as possible even for a small load, but that there is no absolute limit if the load is carried against the body. Common sense should prevail and if a given load causes pain, you have to wait a few more weeks!
-
Static positions, sitting or standing without walking, are poorly tolerated and a source of pain. Frequent change of position is preferable.
Sport:
-
Resuming sports activities should not cause the onset or increase of pain, but early resumption is desirable so as not to lose too much muscle.
-
Brisk walking remains the best sport activity for the back. In case of balance disorders or subjective insecurity, the use of Nordic walking poles is recommended.
-
Climbing the stairs is an excellent exercise, but descending the stairs is less favorable. If an elevator is available, walk up and down by elevator!
-
Swimming is possible on the back and front crawl, but breaststroke should be avoided for 3 months as it increases lumbar lordosis too much.
-
Running is possible from 3 months, but avoiding asphalt. Prefer running in the forest or on a Finnish track, for example.
-
Downhill skiing or snowboarding is possible between 3 and 6 months.
-
Snowshoeing is excellent and can be started after 1 month.
-
The bike can be picked up within one month of the operation. This sport does not strain the back if you use a high speed of rotation and avoid too hard developments. Cycling is an excellent cardiovascular sport for the quadriceps and calves, but it does not strengthen the back or stomach.
-
Sports involving strong dissociated shoulder / pelvis rotations such as tennis or golf should be avoided for at least 6 months.
Work:
-
You are at least on complete sick leave until the postoperative check-up at 3 weeks, then according to your assessment.
-
As a general rule, the average duration of a complete sick leave for this type of intervention is 3 to 4 months. A part-time recovery usually follows this period of total stoppage.
Transport:
-
Car trips should not exceed 30 consecutive minutes in the 1st month. If a longer trip is required, take a break after 30 minutes and walk at least 10 minutes during this break. A longer journey is not only painful, but it increases the risk of deep vein thrombosis (which is already temporarily increased by the operation).
-
The most suitable means of transport is the train . The bus and the plane are possible and better supported than the car.
-
When a journey is feasible on foot, do not take the car!
-
One week before the operation, there is no longer any difference between passenger and driver and you can drive or not depending on your preference.
Night:
-
The prone position is not well tolerated and is not recommended.
-
If there are no breathing problems, a flat lying position is preferred, however a slight angle (10 degrees) is acceptable.
-
The recommended type of mattress is either very hard or "memory" type Tempur
-
While lying on the back, it is necessary to put a cushion under the knees to avoid lumbar hyperlordosis and while lying on the side, it is necessary to put a cushion between the knees to prevent rotation of the pelvis.
Radiological examinations:
-
Your intervention does not contraindicate any subsequent radiological examination. X-rays, a CT-scan, an ultrasound or an MRI are perfectly possible in the event of a medical indication. No special precautions are necessary for these radiological examinations.
Physiotherapy:
-
Physiotherapy is prescribed by medical prescription and is not systematic.
-
In most cases, we assess its indication for control at 3 weeks after the operation.
-
The goals of physiotherapy are:
-
Educational (learn to behave with your back problem)
-
Analgesic (reduce pain)
-
Improvement in proprioception (perception of the body in space), especially for the pelvis and ankles
-
Improved muscle function with reduced strength
-
-
Whenever possible, choose a physiotherapist near your home to avoid a car trip to get there.
.
Various:
-
It is possible to shower with the special dressing that has been applied, but it should be dried well by dabbing afterwards. Do not rub so as not to peel off the dressing and steristrips.
-
It is best to wait 4 days after removing the dressing to take a bath.
-
Physiotherapy in the pool is possible with the shower dressing, but you should not stay in the water for more than 20 minutes.
-
It is possible to resume sex as soon as you get home, but it is better to make your partner work.

